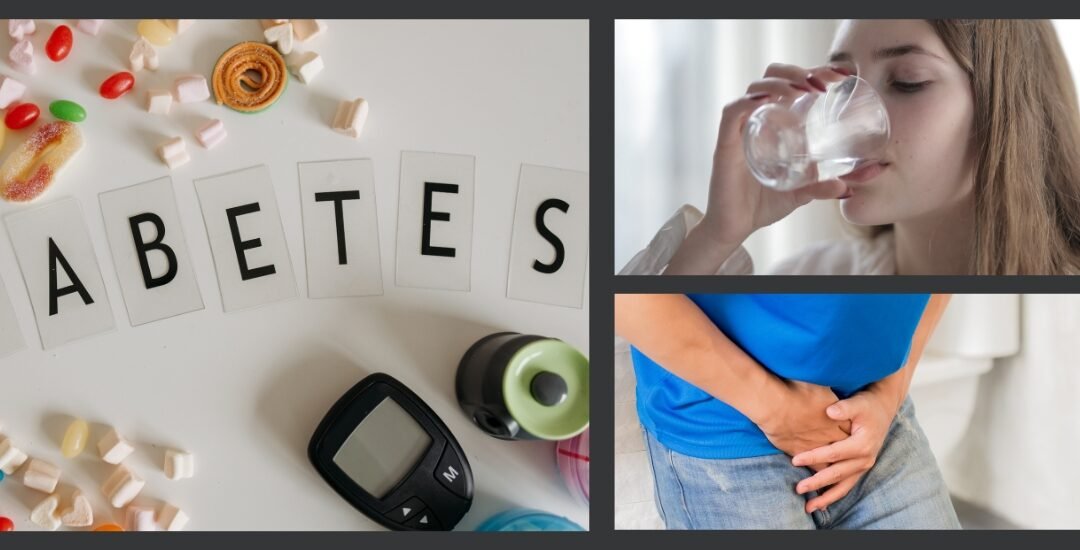
While it shares part of its name with diabetes mellitus, diabetes insipidus is a completely different condition—and one that can become dangerous if left untreated. This rare disorder affects the body’s ability to regulate fluid balance, leading to extreme thirst and excessive urination. Understanding the key diabetes insipidus symptoms is essential for timely diagnosis and treatment.
If you’re frequently thirsty or making constant trips to the bathroom without explanation, it may be more than dehydration. This blog will walk you through the signs, causes, and treatments of diabetes insipidus, and when to seek care.
Table of Contents
- What Is Diabetes Insipidus?
- How It Differs from Diabetes Mellitus
- Key Diabetes Insipidus Symptoms
- Central Diabetes Insipidus Signs
- Nephrogenic Diabetes Insipidus Symptoms
- Causes of Diabetes Insipidus
- How Diabetes Insipidus Is Diagnosed
- Treatment for Diabetes Insipidus
- Managing Fluid Loss in Diabetes Insipidus
- Walk-In Endocrine Evaluation
- When to Seek Medical Attention
- Call to Action
- Final Thoughts
1. What Is Diabetes Insipidus?
Diabetes insipidus (DI) is a condition that disrupts the body’s ability to regulate fluid balance due to problems with the hormone vasopressin, also known as antidiuretic hormone (ADH). When ADH function is impaired, your kidneys can’t retain water effectively, resulting in large volumes of diluted urine.
2. How It Differs from Diabetes Mellitus
Unlike diabetes mellitus, which involves insulin and blood sugar regulation, diabetes insipidus is a water balance disorder. People with DI don’t have high blood sugar. Instead, they experience fluid imbalance symptoms like excessive thirst and urination.
3. Key Diabetes Insipidus Symptoms
The hallmark diabetes insipidus symptoms include:
- Extreme thirst, especially for cold water
- Producing unusually large amounts of urine (polyuria)
- Frequent nighttime urination (nocturia)
- Preference for cold drinks
- Fatigue or dehydration symptoms
In children, DI may also present with delayed growth, irritability, or bedwetting.
4. Central Diabetes Insipidus Signs
Central diabetes insipidus results from damage to the hypothalamus or pituitary gland, affecting ADH production. Signs may appear suddenly and include:
- Sudden, intense thirst
- Constant urination of clear, diluted urine
- Dehydration symptoms like dry skin or low blood pressure
5. Nephrogenic Diabetes Insipidus Symptoms
Nephrogenic diabetes insipidus occurs when the kidneys don’t respond properly to ADH. This can be genetic or acquired due to medications or chronic kidney issues. Symptoms often overlap with central DI but may appear more gradually.
6. Causes of Diabetes Insipidus
The causes of diabetes insipidus vary depending on the type:
- Central DI: Brain injury, tumors, infections, or surgery affecting the pituitary or hypothalamus
- Nephrogenic DI: Inherited genetic mutations or side effects from medications like lithium
- Gestational DI: Rarely occurs in pregnancy due to placental enzyme interference
- Primary Polydipsia: Excessive fluid intake reducing ADH effectiveness
7. How Diabetes Insipidus Is Diagnosed
Diagnosing diabetes insipidus typically involves urine and blood tests to assess fluid concentration, sodium levels, and ADH function. A water deprivation test may be used to observe how the body retains fluids under restricted intake. In cases of suspected central DI, brain imaging such as MRI helps identify abnormalities in the hypothalamus or pituitary gland.
8. Treatment for Diabetes Insipidus
Treatment varies depending on the underlying type of DI. Central DI often responds well to desmopressin, a synthetic version of ADH. Nephrogenic DI management focuses on dietary adjustments, such as reducing salt intake, along with medications like anti-inflammatories or diuretics. Primary polydipsia may benefit from behavioral changes and hydration monitoring.
9. Managing Fluid Loss in Diabetes Insipidus
Managing fluid loss is key to preventing complications. Patients are encouraged to maintain steady fluid intake and watch for signs of dehydration, such as fatigue, dry mouth, or dizziness. Regular monitoring of electrolytes and proper dietary adjustments can help balance hydration and avoid imbalances.
10. Walk-In Endocrine Evaluation
At Walk In PCP, we offer comprehensive walk-in clinic endocrine evaluation services. Whether you’re experiencing unexplained thirst or frequent urination, our providers are equipped to diagnose and manage hormonal conditions like diabetes insipidus.
No appointment is necessary, and timely care can make a significant difference in preventing complications.
11. When to Seek Medical Attention
Don’t ignore the signs you may need care. Seek help if you experience:
- Persistent excessive urination and thirst
- Symptoms of dehydration despite drinking fluids
- Sudden onset of symptoms after head trauma or surgery
Prompt diagnosis and treatment can prevent serious health risks.
12. Call to Action
If you or a loved one is experiencing signs of diabetes insipidus, don’t wait. Visit Walk In PCP, for an immediate endocrine evaluation. Our experienced team offers same-day visits, thorough diagnostics, and customized treatment plans to get your fluid balance and quality of life back on track.
13. Final Thoughts
Recognizing diabetes insipidus symptoms early is the key to managing this rare but impactful condition. With proper evaluation, treatment, and hydration strategies, patients can lead healthy, symptom-controlled lives.
If you or a loved one experience unusual fluid loss or thirst, visit Walk In PCP. Our caring team is here to help you get answers and start appropriate care.
Disclaimer
This blog is for informational purposes only and does not substitute for professional medical advice. Always consult your healthcare provider for personalized diagnosis and treatment options.