It’s vital for you to be aware of the signs and symptoms of prostate cancer, as early detection can significantly improve your treatment outcomes. You may experience changes such as difficulties with urination, blood in urine, or persistent pain in the lower back. Noticing these symptoms early on allows you to seek medical attention promptly, giving you the best chance for a favorable prognosis. Staying informed and proactive about your health can be your best ally in combating this condition.
Recognizing Early Signs: What Your Body Might be Telling You
Changes in Urination Patterns
One of the earliest signs you may notice in relation to prostate health is a shift in your urination patterns. If you find yourself needing to urinate more frequently, especially at night, or if there is an urgent need to go that seems disproportionate to your fluid intake, this can be a warning signal. You might also experience a decrease in the strength of your urine stream or even a sense of incomplete bladder emptying. These symptoms arise because an enlarged prostate can compress the urethra, leading to obstructed urinary flow.
Moreover, painful urination, known as dysuria, can accompany these changes and might indicate irritation. The presence of blood in your urine or semen should prompt you to seek medical attention immediately, as these can be associated with more advanced prostate conditions, including cancer. Awareness of these subtle changes can empower you to take the necessary actions sooner rather than later.
Unexplained Pain in the Lower Back and Hips
Feeling discomfort or persistent pain in your lower back and hips can often be overlooked as a benign issue, especially in an aging population. However, this pattern of pain could signify that there’s more going on, particularly concerning your prostate health. Prostate cancers can metastasize or spread to nearby bones, leading to pain that is often described as dull or achy. You might notice this pain worsening with activity or even at rest, and it may also disrupt your sleep patterns, further indicating that it’s worth discussing with your healthcare provider.
Unlike typical back pain that may result from muscle strain or poor posture, prostate-related pain usually does not improve with routine home remedies or over-the-counter pain relief medications. Being attentive to these changes in your body can be the first step toward early diagnosis, which is important in improving treatment outcomes and maintaining quality of life.
Advanced Symptoms: When Prostate Cancer Progresses
As prostate cancer advances, you may experience a range of additional symptoms that indicate a progression of the disease. These advanced symptoms often result from the cancer spreading to other parts of the body, leading to complications that can significantly affect your quality of life. If you notice any of these signs, it is crucial to consult with your healthcare provider for appropriate assessment and intervention.
- Bone pain or weakness
- Unexplained weight loss
- Extreme fatigue or weakness
- Difficulty urinating or blood in urine
- Painful ejaculation or sexual dysfunction
- Swelling in the legs or pelvic area
| Physical Signs | Description |
|---|---|
| Weight Loss | Unintentional weight loss can indicate that the body is fighting cancer, as it often leads to a loss of appetite and changes in metabolism. |
| Fatigue | A deep sense of tiredness is common, which may not improve with rest, reflecting the body’s struggle with disease progression. |
Physical Signs: Weight Loss and Fatigue
Weight loss that occurs without any deliberate change in diet or exercise can be alarming. In advanced prostate cancer, your body’s metabolic processes may become disrupted, resulting in significant weight loss. This loss is often accompanied by a decreased appetite, making it challenging to maintain nutrition. Additionally, you might find that you have little energy or stamina, despite getting rest. This fatigue can be debilitating, impacting your daily activities and overall well-being.
Alongside weight loss, fatigue may manifest as an overwhelming sense of tiredness or lack of motivation to engage in previously enjoyable activities. Studies show that nearly 40% of men with advanced cancer report experiencing significant fatigue. This persistent exhaustion can stem from various factors, including the body’s response to cancer, treatments such as chemotherapy, and emotional stress related to the diagnosis. Understanding these symptoms allows you to seek appropriate support and resources, potentially improving your quality of life.
Emotional and Psychological Impact: Anxiety and Depression
The emotional toll of a prostate cancer diagnosis can be profound, leading to heightened levels of anxiety and depression. You may find yourself grappling with worries about mortality, changes in sexual function, and the financial implications of your treatment. Anxiety often manifests through physical symptoms such as rapid heartbeat, difficulty concentrating, or restlessness. This psychological burden can create a feedback loop where anxiety exacerbates physical symptoms of the disease, such as fatigue and pain.
Depression can also set in, leading to feelings of hopelessness or a loss of interest in once-loved activities. Reports suggest that about 25% of individuals with cancer experience clinical depression, making it crucial to acknowledge these feelings and seek assistance. Therapy, support groups, and medication may provide you with relief from the emotional strain of coping with cancer. You are not alone; it is vital to explore resources that can support both your mental and emotional health throughout this challenging journey.
The Role of Screening: Why It’s Critical
Engaging in regular screening for prostate cancer can make a significant difference in outcomes, as early detection greatly enhances treatment options and survival rates. Studies have shown that the chances of successful treatment are substantially higher when the cancer is caught in its earlier stages, reducing the likelihood of requiring more aggressive therapies later on. Most experts believe that discussing the potential benefits and risks of screening with your healthcare provider is an crucial step in managing your overall health. This conversation can provide a tailored approach based on your individual risk factors, such as age, family history, and ethnicity.
Guidelines for Regular Check-ups
The standard recommendations for prostate cancer screenings typically start at age 50 for most men, although African American men and those with a family history of prostate cancer may need to begin discussions about screening as early as age 45. Regular check-ups should include a discussion about your current health status and any new symptoms you may have experienced. Following these guidelines not only puts you in a proactive position regarding your health but also allows for earlier detection of any irregularities that could indicate a problem.
The Importance of PSA Testing
Prostate-specific antigen (PSA) testing has revolutionized the early detection of prostate cancer. This blood test measures the level of PSA in your blood, with higher levels often associating with an increased risk for prostate cancer. While PSA testing can sometimes lead to false positives, the information it provides remains valuable in conjunction with further diagnostic procedures. Timely PSA tests can uncover issues before they become advanced, facilitating decisions about monitoring, biopsies, or potential treatment options.
Moreover, many studies underline that men who undergo regular PSA testing experience lower mortality rates from prostate cancer as compared to those who do not. Over time, it has shown to play a pivotal role in aiding men to make informed choices regarding their health. You might consider talking to your doctor about how frequently you should get tested based on your personal health profile, especially as current guidelines may vary based on emerging research and trends in prostate health management.
Connecting the Dots: Risk Factors and Lifestyle Choices
Understanding the risk factors and lifestyle choices related to prostate cancer can empower you in making informed health decisions. Certain variables are more likely to elevate your risk, including age, ethnicity, and family history. It’s vital to recognize that these factors are interconnected and can significantly influence your overall risk profile. Moreover, lifestyle choices, such as diet and physical activity, can also play a crucial role in your susceptibility.
- Age: The risk of prostate cancer increases significantly after age 50.
- Ethnicity: African American men are at a higher risk than men of other ethnicities.
- Family History: A family history of prostate cancer can double your risk.
- Obesity: Being overweight can increase your risk of developing aggressive forms of prostate cancer.
- Diet: High-fat diets and a lack of fruits and vegetables may link to a greater risk.
Thou must stay vigilant about how these risk factors intertwine with your life choices; proactive efforts could be key to maintaining your health.
Genetics and Family History
Your genetic makeup plays a pivotal role in your risk of developing prostate cancer. If you have a father or brother diagnosed with this condition, your risk of developing it doubles compared to those without a family history. Certain inherited mutations, especially in the BRCA1 and BRCA2 genes, have also been linked to prostate cancer. It’s estimated that about 5-10% of all prostate cancer cases are hereditary, making understanding your family medical history vital for early detection and prevention.
Having a family member affected by prostate cancer doesn’t guarantee you’ll develop the disease, but it puts you into a higher-risk category. Genetic counseling and regular screenings are recommended for men with a family history, as identifying risk can enhance early detection efforts.
Diet and Its Potential Impact
Your dietary choices may have a considerable impact on prostate cancer risk. Studies suggest that diets high in red meat and dairy products may elevate your chances, whereas a diet rich in fruits, vegetables, and healthy fats, such as omega-3 fatty acids, could potentially provide a protective effect. Specific nutrients, like lycopene found in tomatoes, and selenium, may be beneficial in lowering the risk.
Incorporating a variety of colors on your plate isn’t just visually appealing but nutritionally advantageous. Foods dotted with antioxidants, such as berries and leafy greens, may aid in reducing inflammation and boosting your immune system. A mindful approach to your calorie intake and embracing vegetarian or Mediterranean-style diets could play a significant role in mitigating health risks associated with prostate cancer, paving the way for a healthier lifestyle.
Navigating Your Next Steps: What to Do If You Suspect Prostate Cancer
Experiencing unusual symptoms or having risk factors associated with prostate cancer can be daunting. Connecting with your healthcare provider promptly can make all the difference. They can offer clarity on your symptoms, recommend diagnostic tests, and guide you through the necessary follow-up. Early detection plays a significant role in treatment success, so acting quickly can ensure that you receive appropriate care and intervention as needed.
Talking to Your Doctor: Key Questions to Ask
Engaging in an open dialogue with your doctor about prostate cancer is vital for your understanding and peace of mind. You might want to ask about your specific symptoms and how they relate to prostate health. Questions like, “What tests will I need to take?” or “What do the results mean for my overall health?” can offer invaluable insight. Additionally, inquire about the implications of family history, with questions such as, “Given my family history, am I at greater risk for prostate cancer?” This provides context and allows your doctor to tailor their approach to your situation.
Don’t hesitate to investigate deeper into potential treatment options should a diagnosis occur. Asking, “What treatment methodologies are available, and how effective are they?” along with questions about side effects and lifestyle adjustments can better equip you for your next steps. Being proactive in these discussions not only empowers you but also lays the groundwork for a collaborative relationship with your healthcare provider.
Preparing for Diagnostic Tests and Procedures
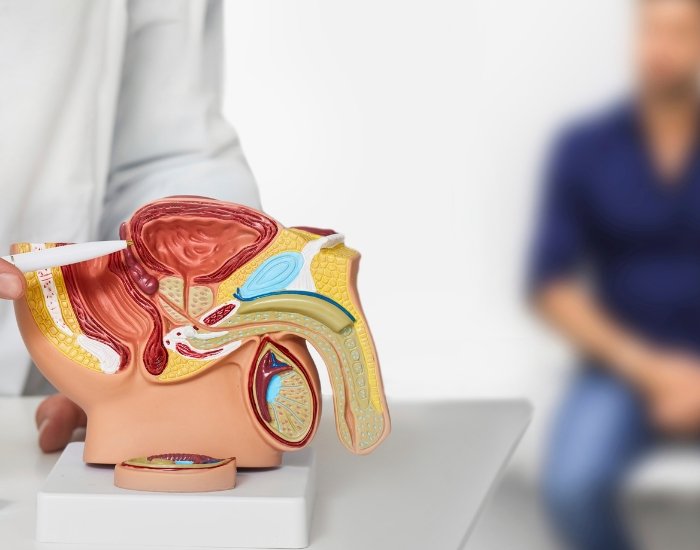
Arriving prepared for diagnostic tests can alleviate some of the anxiety associated with the process. Your doctor may recommend tests such as a prostate-specific antigen (PSA) blood test or a digital rectal exam (DRE). Familiarizing yourself with these tests and understanding their purposes will help ease any apprehensions. For instance, the PSA test measures the levels of a specific protein that can signal prostate issues, while the DRE allows for a physical assessment of the prostate by your doctor.
Preparing also involves the practicalities of what to expect on the day of the test. You may be advised to avoid certain medications or supplements prior to your appointment, as they can affect the results. Ensuring that you have personal identification, insurance information, and an understanding of your medical history can facilitate a smoother experience. Keeping a journal of your symptoms can also be advantageous, as sharing this information with your healthcare provider aids in pinpointing issues and discusses results more effectively.
To Wrap Up
Now that you are informed about the signs and symptoms of prostate cancer, it’s important to stay vigilant about your health. You should be aware that early detection significantly increases the chances of successful treatment. If you experience any of the symptoms discussed, such as frequent urination, discomfort during urination, or unexplained weight loss, you must consult your healthcare provider for further evaluation. Your awareness and proactive approach can play a vital role in your health journey.
Additionally, it’s beneficial for you to discuss with your doctor your personal risk factors for prostate cancer, including family history and age. Regular check-ups and screenings can help you monitor your prostate health effectively. By staying informed and engaged with your health, you can take meaningful steps toward early detection and treatment, ultimately contributing to better outcomes for yourself.