It’s crucial to understand how long a respiratory infection can last, as this can significantly affect your daily life and recovery process. Typically, most mild infections resolve within one to two weeks, but more severe cases can linger for up to three weeks or longer. Factors such as your overall health, age, and the specific type of infection can influence your recovery time. By identifying symptoms early and taking appropriate care, you can potentially shorten the duration of your illness and return to your normal routine sooner.
The Stages of Respiratory Infections: What to Expect
Initial Symptoms and Duration
Typically, respiratory infections begin with initial symptoms that can catch you off guard. You might notice sore throat, runny or stuffy nose, and mild cough as early markers of your infection. The onset of these symptoms can happen quite suddenly, often within 1 to 3 days after exposure to the virus. Most individuals can expect these initial symptoms to persist for about 3 to 7 days, making it vital to monitor your condition closely to determine if it progresses into something more severe.
During this early phase, your body is actively fighting off the infection. You may also experience mild fever or general fatigue, which can further contribute to your discomfort. Taking notice of how these initial symptoms evolve can provide valuable insight into your overall health status and help you make informed decisions about seeking medical attention if necessary.
Peak Illness Phase: Timeline and Intensity
The peak illness phase usually occurs about 3 to 5 days after the onset of initial symptoms. This is when you might feel the most unwell, as your body reacts to the pressing infection. Symptoms may escalate to include more severe coughing, pronounced congestion, and even shortness of breath or wheezing. At this stage, you may find daily activities challenging, especially if your respiratory function is impaired. Understanding this timeline can help you prepare mentally for the intensity of your illness, which can have a profound impact on your daily routine.
During the peak of the infection, your immune system is engaged in a full-scale defense, which can sometimes lead to secondary symptoms such as further body aches or prolonged fatigue. Keeping yourself well-hydrated and resting significantly can aid in alleviating some discomfort. If symptoms worsen or do not start to abate after a few days, it’s advisable to consult a healthcare professional for further guidance on managing your condition effectively.
Factors Influencing Recovery Times: Beyond the Infection Itself
Recovery from a respiratory infection can vary widely, often influenced by various factors that extend beyond the infection itself. Those factors include your age, overall health, specific type of infection, and any pre-existing conditions. Environmental influences such as air quality and access to healthcare can play significant roles in your recovery trajectory. Understanding how these elements intertwine can help you manage your health more effectively and set realistic expectations for your recovery time. You might find yourself feeling improved sooner than initially expected, or, conversely, your recovery might be prolonged due to unforeseen complications.
Another factor that can significantly affect your recovery timeline is how promptly you sought treatment. Early intervention in the form of medication, rest, and hydration can shorten the duration of symptoms. Following your healthcare provider’s advice and taking prescribed medications regularly help mitigate the effects of the infection, potentially leading you to a faster resolution. The timeliness of treatment combined with addressing other health determinants makes all the difference in how long a respiratory infection lasts in your experience.
Age and Overall Health
Your age and overall health status play vital roles in determining how long a respiratory infection persists. Generally, older adults, particularly those over 65, may experience prolonged symptoms due to a natural decline in immune function that comes with aging. Moreover, if you have underlying conditions such as asthma, diabetes, or heart disease, the recovery may take longer since your body is already working harder to combat existing health challenges while fighting off the infection. For younger, healthy individuals, symptoms often resolve more swiftly, typically within a week or two.
Lifestyle factors also contribute significantly. If you have a balanced diet, regular exercise, and good sleep hygiene, these elements can bolster your immune system and expedite recovery. Conversely, poor nutrition, high-stress levels, and lack of physical activity can hinder your body’s ability to heal. Always remember that maintaining a healthy lifestyle not only enhances your overall well-being but also supports a more effective defense against respiratory infections.
Specific Viral vs. Bacterial Infections
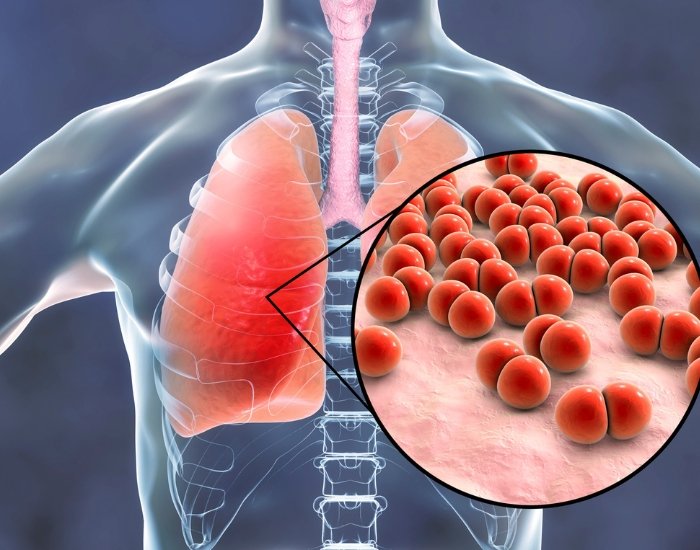
When considering recovery duration, the distinction between viral and bacterial infections is imperative. Viral respiratory infections, such as the common cold or influenza, usually resolve within a week to ten days. In some cases, lingering symptoms like a cough or fatigue may persist for several weeks. Bacterial infections, on the other hand, tend to require targeted antibiotic treatment and can lead to more severe complications if not promptly addressed. In such cases, your recovery may extend several weeks following the initiation of treatment, particularly if complications like pneumonia arise.
Additionally, a common misconception is that all respiratory infections follow the same course; this is far from the truth. For instance, infections caused by bacteria often have abrupt symptom onset and can present with high fever, severe fatigue, and significant respiratory distress. Viral infections may develop gradually with milder symptoms initially, which can lead to misunderstandings regarding their severity. Recognizing the signs and understanding the different types of infections can help you seek appropriate treatment sooner, ultimately impacting the duration of your illness.
The Role of Treatment: Does It Really Make a Difference?
Treatment for respiratory infections can significantly impact both the duration and severity of your symptoms. While many mild respiratory infections may resolve on their own, effective treatment can alleviate discomfort and speed up recovery. Antibiotics may be necessary in the case of bacterial infections; however, it’s worth noting that they are ineffective against viral infections, which are responsible for the majority of respiratory infections you encounter. The impact of treatments is very much dependent on factors such as the type of infection and your overall health status.
In some cases, strong medications such as corticosteroids may be prescribed to reduce inflammation in the lungs, particularly if you have conditions like asthma or chronic obstructive pulmonary disease (COPD). Over-the-counter treatments can also play a significant role. Managing your symptoms effectively can ease your overall experience, allowing you to return to normal activities faster. The right combination of treatments and self-care strategies helps many individuals successfully navigate through the discomfort of respiratory infections.
Over-the-Counter Remedies and Their Efficacy
Over-the-counter medications can provide relief from the symptoms associated with respiratory infections. Antihistamines may help control sneezing and runny nose, while decongestants facilitate easier breathing by reducing nasal swelling. Pain relievers like ibuprofen and acetaminophen are beneficial for managing fever and body aches, common accompaniments of infections. That said, the efficacy of these remedies varies from person to person; some may notice significant improvements in a short time, while others might require additional measures.
While these remedies can alleviate discomfort, they do not necessarily shorten the duration of the infection itself. For example, studies have shown that decongestants can relieve nasal congestion but do not significantly affect the overall duration of your illness. As a result, focusing on symptom management can enhance your comfort level, but you should also pay attention to recovery processes, including rest and hydration.
When to Seek Professional Help
Recognizing the right time to consult with a healthcare provider can make all the difference in your healing process. If your symptoms persist beyond the typical duration—usually around 7 to 10 days for a common cold—or worsen alarmingly, it’s advisable to seek professional assistance. Additionally, look out for signs like high fever, chest pain, difficulty breathing, or wheezing, which could indicate more serious conditions requiring immediate evaluation.
A healthcare professional can perform necessary examinations to determine whether your infection is bacterial or viral. For instance, if you exhibit severe coughing alongside mucus that has changed in color or consistency, your healthcare provider might conduct tests to identify the underlying cause. Early intervention can often lead to better outcomes, ensuring that you manage your infection effectively and prevent complications that may prolong your discomfort.
Long-term Effects: When Recovery is Not Complete
Some individuals may experience lingering symptoms after recovering from a respiratory infection. These long-term effects can vary widely, impacting your quality of life. A persistent cough, for instance, could last for several weeks or even months after the initial infection has cleared. This lingering cough is often due to residual inflammation within your lungs or airways, a situation referred to as post-infectious cough syndrome. In some cases, fatigue and shortness of breath may also persist, which can notably hinder daily activities.
Post-Infection Complications
Post-infection complications can manifest in various ways, complicating your recovery. You may notice an increase in respiratory symptoms, such as wheezing or chest tightness, even after the acute phase of the infection has passed. This is sometimes a sign of reactive airway disease, where your airways remain sensitive long after the infection has resolved. Additionally, individuals with preexisting health conditions may find that their symptoms exacerbate, leading to increased doctor visits or additional treatments. For those at higher risk, such as the elderly or those with chronic respiratory conditions, these complications can foster a cycle of illness that is difficult to break.
Chronic Conditions: The Shadow of Respiratory Infections
In some situations, a respiratory infection can trigger or exacerbate chronic conditions. Conditions such as asthma or chronic obstructive pulmonary disease (COPD) can become more pronounced following infections. If you have asthma, for example, an infection may lead to an increase in asthma attacks as your respiratory system becomes hyper-responsive. This phenomenon emphasizes the necessity for continuous management of preexisting conditions even after you feel better.
Medical literature highlights that individuals who experienced severe respiratory infections, like pneumonia or COVID-19, are at an increased risk for developing long-term complications, including pulmonary fibrosis — a condition that causes scarring in the lungs. This scarring can make breathing increasingly difficult over time, demonstrating the critical need for follow-up care and monitoring. Understanding the connection between your respiratory history and potential future risks offers an important roadmap for maintaining health.
Social and Economic Impacts: The Hidden Costs of Respiratory Illnesses
Workplace Productivity Loss
Absenteeism due to respiratory infections can significantly impact workplace productivity, with studies showing that employees miss an average of 4 to 5 days of work for each illness episode. This loss not only affects individual productivity but also places strain on colleagues who must pick up the slack. You may also be aware that employers face the burden of reduced team morale and project delays, which can lead to substantial economic losses. The total cost of absenteeism related to respiratory illnesses in the workforce can reach staggering figures not only in lost wages but also in decreased organizational performance.
When employees return to work before fully recovering, known as “presenteeism”, the effects can be equally damaging. You may notice that individuals working under these circumstances are less focused, more prone to errors, and less efficient. This state can ultimately lead to decreased quality of work and an increased likelihood of further health complications that might result in additional absenteeism down the line. The productivity costs can thus ripple through the entire organization, elevating the risk of long-term economic repercussions.
Public Health Considerations
Beyond immediate personal and workplace impacts, respiratory infections pose a significant threat to public health systems. The increased need for healthcare services during peak infection periods can overwhelm hospital resources and already strained healthcare infrastructures. For example, during the flu season, emergency room visits can spike by as much as 46%, further highlighting the need for effective public health strategies. Your local health department may be compelled to implement measures such as vaccination campaigns or community awareness programs in an attempt to mitigate the spread of infections and alleviate strain on healthcare resources.
Proper management of respiratory infections requires collaboration between health officials, healthcare providers, and the community. You may see initiatives aimed at improving vaccination rates, promoting hygiene practices, and educating the public on recognizing early symptoms. Enhanced surveillance for outbreaks can guide public health interventions that effectively reduce transmission and protect vulnerable populations, ultimately leading to better community health and resilience against future respiratory illness outbreaks.
Conclusion
Considering all points, the duration of a respiratory infection typically ranges from a few days to a couple of weeks, depending on the type and severity of the infection. If you are experiencing mild symptoms, you might find that your body naturally recovers within a week or so. On the other hand, if the infection is more severe or if you have underlying health conditions, it could take longer for you to feel completely better. Maintaining proper hydration, rest, and nutrition can play a significant role in supporting your recovery during this period.
It is also important to note that some symptoms, like a lingering cough, may last even after you start to feel better. If you find that your symptoms persist beyond two weeks or worsen, it is advisable for you to consult a healthcare professional. Understanding the expected duration of your respiratory infection empowers you to manage your recovery effectively, while also emphasizing the importance of listening to your body as it heals.